Pleural mesothelioma is a rare cancer that develops in the pleura, the thin tissue surrounding the lungs. It often results from prolonged asbestos exposure, making it a significant occupational health concern. Understanding its progression is vital for improving treatment outcomes. Early-stage tumors allow for intervention, while advanced stages demand comprehensive care, as shown below:
| Stage | Description | Treatment Implications |
|---|---|---|
| 1 | Localized tumors | Early intervention possible |
| 2 | Localized tumors | More aggressive treatment may help |
| 3 | Spread to nearby tissues | Comprehensive treatment required |
| 4 | Metastatic disease | Palliative care becomes the focus |
Key Takeaways
- Breathing in asbestos is the main cause of pleural mesothelioma. Knowing this danger helps prevent and find it early.
- Small tumors in early stages are easier to treat. Spotting signs early helps doctors act quickly.
- New imaging tools and biomarkers make diagnosis better. Using these tools helps find and treat it sooner.
Pathogenesis of Pleural Mesothelioma

Asbestos Exposure and Disease Development
Asbestos exposure remains the primary cause of pleural mesothelioma. When asbestos fibers are inhaled, they lodge in the pleura, triggering harmful biological processes.
- The fibers generate reactive oxygen species (ROS), which damage DNA and cause mutations.
- They interfere with the cell cycle, leading to chromosomal abnormalities during cell division.
- Asbestos traps carcinogenic molecules on its surface, increasing cancer risk.
- It also stimulates mesothelial cells and macrophages to release inflammatory cytokines, promoting tumor growth.
These processes create a toxic environment in the pleura, setting the stage for cancer development.
Non-Asbestos-Related Causes
Although asbestos is the leading cause, other factors can contribute to pleural mesothelioma. Environmental and occupational risks include:
| Risk Factor | Description |
|---|---|
| Zeolite (erionite) | An asbestos-like mineral fiber that can induce mesothelioma. |
| SV-40 viruses | Viruses that may play a role in the development of mesothelioma. |
| Recurrent infections | Chronic infections that could contribute to mesothelioma risk. |
| Genetic predisposition | Inherited factors that may increase susceptibility to mesothelioma. |
| Innovative nanomaterials | Research is ongoing to determine if nanotubes could be carcinogenic. |
These factors highlight the need for broader research into non-asbestos-related causes.
Genetic and Molecular Pathways
Genetic mutations and molecular changes play a critical role in pleural mesothelioma. Deletions in specific chromosome regions, such as 1p, 3p, 6q, 9p, 13q, 15q, and 22q, are common. Tumor suppressor genes like CDKN2A, NF2, and BAP1 are frequently altered. CDKN2A deletions disrupt cell-cycle regulation, leading to uncontrolled cell growth. Mutations in NF2 and BAP1 further contribute to tumor development.
Epigenetic changes, such as hypermethylation of p16INK4A or p19ARF, often precede mesothelioma. These alterations affect gene regulation, increasing cancer risk. CDKN2A, the most altered gene in pleural mesothelioma, encodes inhibitors of cyclin-dependent kinases. Its deletion promotes aggressive tumor growth, making it a key target for future treatments.
Progression of Pleural Mesothelioma
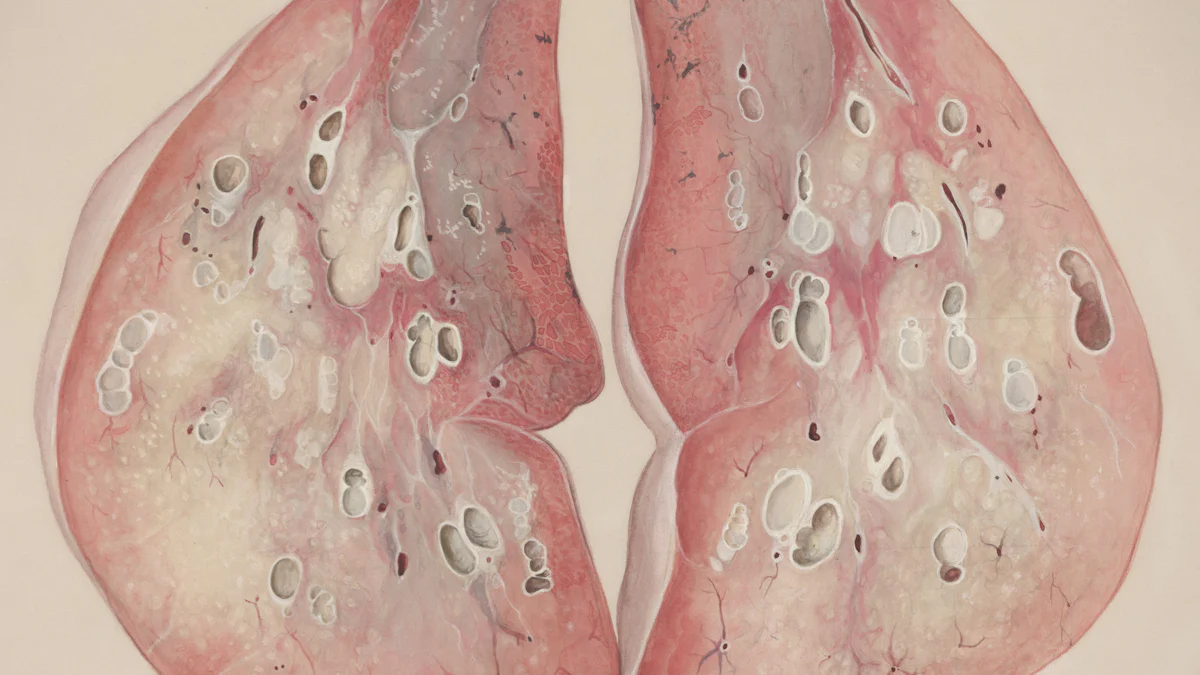
Tumor Growth in the Pleura
Tumor growth in the pleura begins when mesothelial cells undergo malignant transformation. These cells form abnormal clusters that gradually expand within the pleural lining. Several factors influence the rate of tumor growth:
- Clinical characteristics, including the patient’s age, gender, and overall health.
- The intensity and duration of asbestos exposure, with higher levels linked to more aggressive tumors.
- Histological subtype, where the epithelioid subtype grows slower and offers a better prognosis compared to nonepithelioid types.
As the tumor enlarges, it thickens the pleura and restricts lung movement. This process often leads to symptoms such as chest pain, shortness of breath, and persistent coughing.
Spread to Nearby Tissues and Organs
Pleural mesothelioma spreads beyond the pleura as the disease progresses. Tumor cells invade nearby tissues and organs, disrupting their function. Commonly affected areas include:
| Organ/Tissue | Description |
|---|---|
| Liver | A frequent site of metastasis. |
| Adrenal Glands | Often impacted by tumor spread. |
| Kidneys | Another organ commonly involved. |
| Opposite Lung | Frequently affected by the disease. |
This spread, known as metastasis, complicates treatment and worsens the prognosis. Early detection remains critical to limiting the extent of this progression.
Systemic Effects and Complications
Advanced pleural mesothelioma causes systemic effects that impact the entire body. Patients often experience weight loss, fatigue, and anemia due to the cancer’s metabolic demands. The disease can also lead to pleural effusion, where fluid accumulates in the pleural cavity, further impairing lung function. In severe cases, the cancer triggers paraneoplastic syndromes, which result from the release of tumor-derived substances. These complications highlight the importance of comprehensive care to manage both local and systemic effects.
Diagnostic Advancements in Pleural Mesothelioma
Imaging Techniques
Advancements in imaging techniques have significantly improved the diagnosis of pleural mesothelioma. Each method offers unique benefits for identifying and assessing the disease:
| Imaging Technique | Effectiveness |
|---|---|
| Transthoracic Ultrasonography | Best for visual guidance in pleural puncture and assessing pleura with effusion. |
| CT | Best for judging tumor extent and detecting lymph node metastases. |
| MRI | Best for determining tumor invasion into diaphragm or chest wall. |
| PET | Greater sensitivity for detecting distant metastases. |
| VATS | Sensitivity 95%-98%, specificity 100% for diagnosing pleural mesothelioma. |
Emerging technologies like breath testing have also shown promise. These tests analyze volatile organic compounds (VOCs) to differentiate between benign and malignant pleural diseases. Sensitivity and specificity for distinguishing pleural mesothelioma from healthy controls range from 0.62–0.96 and 0.22–1.0, respectively. Artificial intelligence further enhances imaging by performing volumetric tumor analysis on CT scans, aligning closely with radiologists’ assessments.
Biomarkers for Early Detection
Biomarkers play a crucial role in detecting pleural mesothelioma at earlier stages. MESOMARK® remains the only FDA-approved biomarker test. However, ongoing research explores combinations of biomarkers to improve diagnostic accuracy. For example:
| Biomarker Combination | AUCROC Value |
|---|---|
| IL6–osteopontin–SMRP | 0.945 |
| IL6–osteopontin–desmin | 0.950 |
| SMRP–osteopontin–IL6–vimentin | 0.960 |
Despite these advancements, no biomarkers have been validated for routine clinical use. Researchers continue to investigate non-invasive methods to enhance early detection.
Molecular Diagnostic Tools
Molecular diagnostic tools provide precise methods for identifying pleural mesothelioma. These tools include:
- Enzyme-linked immunosorbent assays (ELISAs) for protein studies.
- Proteomics-based approaches using mass spectrometry for biomolecule identification.
- RNA evaluation through extraction, quantification, and PCR amplification.
Specific markers like Wilms’ tumor 1 (WT1) protein and BAP1 help distinguish mesothelioma from other cancers. For example, WT1 combined with cytokeratins achieves 97.7% specificity in differentiating sarcomatoid carcinoma from sarcomatoid mesothelioma. Additionally, breath analysis has emerged as an experimental diagnostic tool, reflecting ongoing innovation in this field.
Treatment Options for Pleural Mesothelioma
Surgery and Its Role
Surgery plays a critical role in managing pleural mesothelioma, especially in early stages. The goal is to remove as much tumor tissue as possible, although complete resection is rarely achievable. Two primary surgical procedures are commonly used:
| Procedure Type | 5-Year Survival Rate | Local Recurrence Rate | Mortality Rate |
|---|---|---|---|
| Extrapleural Pleuropneumectomy (EPP) | 45% (early-stage) | 0% – 37% | 3.4% – 10% |
| Pleurectomy/Decortication (P/D) | N/A | 2.5% – 5.9% | 1.5% – 5% |
EPP involves removing the affected lung, pleura, diaphragm, and pericardium. While it offers a chance for extended survival, it carries high morbidity and no significant survival advantage. P/D, which spares the lung, has a lower mortality rate but a higher risk of local recurrence. These limitations highlight the need for multimodal approaches to improve outcomes.
Chemotherapy and Radiotherapy
Chemotherapy and radiotherapy remain essential components of pleural mesothelioma treatment. Chemotherapy, particularly the combination of cisplatin and pemetrexed, shows modest effectiveness in slowing disease progression. However, randomized trials have not consistently demonstrated significant survival benefits. Radiotherapy primarily serves a palliative role, alleviating symptoms and reducing local recurrence.
Multimodal treatment, combining surgery, chemotherapy, and radiotherapy, offers the best outcomes. Despite this, the five-year survival rate remains low at approximately 10%. Adjuvant therapies often fail to prevent recurrence, and radiotherapy’s toxicity limits its use near vital organs like the lungs.
Emerging Therapies
Emerging therapies provide hope for improving pleural mesothelioma outcomes. Immunotherapy enhances the immune system‘s ability to target cancer cells. Drugs like Opdivo® (nivolumab) and Yervoy® (ipilimumab) have shown promise, with FDA approval for pleural mesothelioma in 2020. CAR T-cell therapy programs T-cells to attack mesothelioma cells directly. Checkpoint inhibitors, such as Keytruda® (pembrolizumab), block proteins that hinder immune responses.
Gene therapy represents another innovative approach. It aims to repair or replace faulty genes responsible for cancer development. Techniques include introducing healthy genes or “suicide genes” to destroy cancer cells. These advancements, while still experimental, offer potential breakthroughs in treating this aggressive disease.
Understanding pleural mesothelioma involves recognizing its complex pathogenesis and progression.
- Asbestos exposure remains a primary cause, inducing proto-oncogenes and DNA damage.
- Tumor growth and systemic effects worsen prognosis.
- Diagnostic advancements, including AI and biomarkers, improve early detection.
Ongoing research into genes and proteins promises innovative tools for earlier diagnosis and effective treatments.
FAQ
What is the primary cause of pleural mesothelioma?
Asbestos exposure is the leading cause. Inhaled fibers lodge in the pleura, causing inflammation, DNA damage, and mutations that lead to cancer development.
Can pleural mesothelioma occur without asbestos exposure?
Yes, non-asbestos causes include genetic predisposition, environmental factors like zeolite exposure, and chronic infections. Research continues to explore these alternative risk factors.
How is pleural mesothelioma diagnosed?
Doctors use imaging techniques like CT scans, biomarkers such as MESOMARK®, and molecular tools like ELISAs to confirm the diagnosis and assess disease progression.
