Malignant Mesothelioma Treatment & Asbestos Cancer Claims: Science-Backed Survival Strategies
The lethal link between asbestos exposure and malignant mesothelioma is undeniable – but new molecular therapies and legal compensation options are rewriting survival odds. Inhaled asbestos fibers trigger NF2 gene mutations in 70% of cases, accelerating tumor growth through disrupted Hippo signaling pathways. For the 3,000 Americans diagnosed yearly, combining immunotherapy breakthroughs (like Keytruda trials) with asbestos trust fund claims can fund life-extending care.
Critical Steps to Secure Compensation and Survival
Asbestos Exposure Proof = Legal Claims + Treatment Access
Document workplace/consumer product history (e.g., shipyard workers, insulation installers) to qualify for both clinical trials and mesothelioma lawsuit settlements averaging $1.2M.
Target BAP1/NF2 Mutations
Ask oncologists about genetic testing – drugs like ADI-PEG20 show 43% progression-free survival in BAP1-deficient patients.
Dual-Action Legal-Medical Strategy
Leading cancer centers (e.g., MD Anderson) partner with asbestos attorneys to fast-track compensation for experimental therapies like Tumor Treating Fields.
Why Asbestos History Dictates Your Cancer Battle
From workplace risks to legal recourse
The 20-50 year latency period means 89% of mesothelioma cases trace back to occupational asbestos exposure. Even short-term contact (e.g., 6-month construction work) qualifies for lawsuits against negligent employers. Proving exposure via:
Employment Records
Attorneys subpoena payroll data from closed factories.
Product Identification
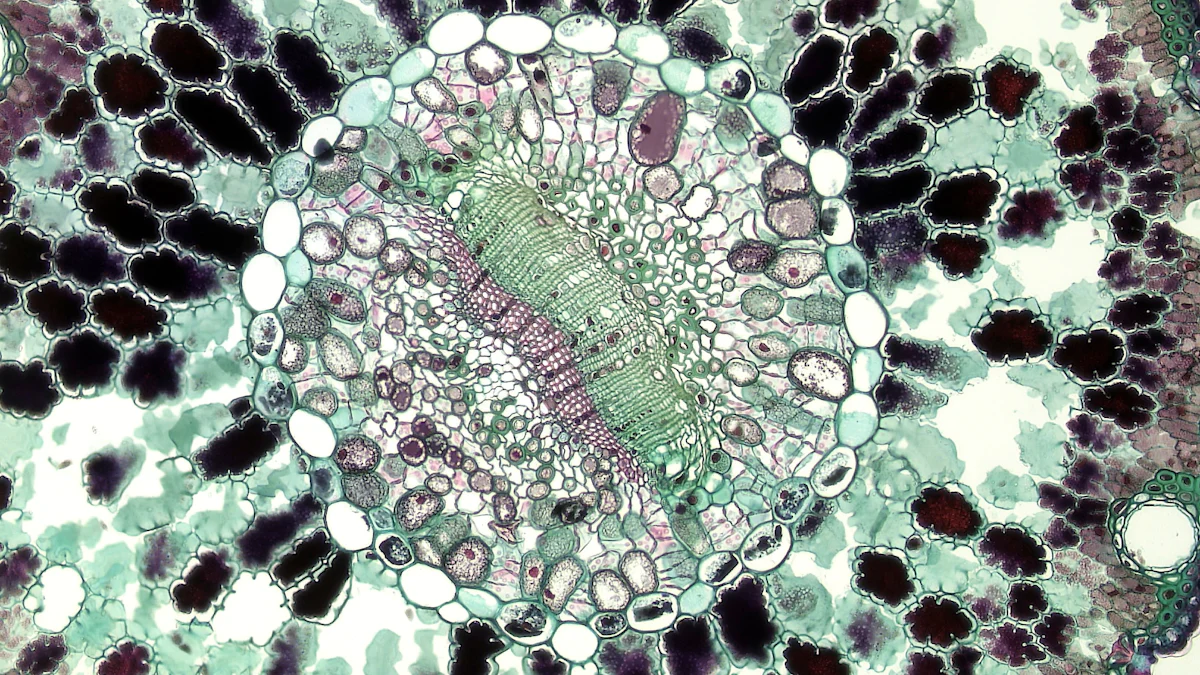
Microscopic fiber analysis matches your lung tissue to specific asbestos products.
VA Benefits
Veterans exposed in Navy shipyards get priority clinical trial access.
Diagnostic and Therapeutic Hurdles
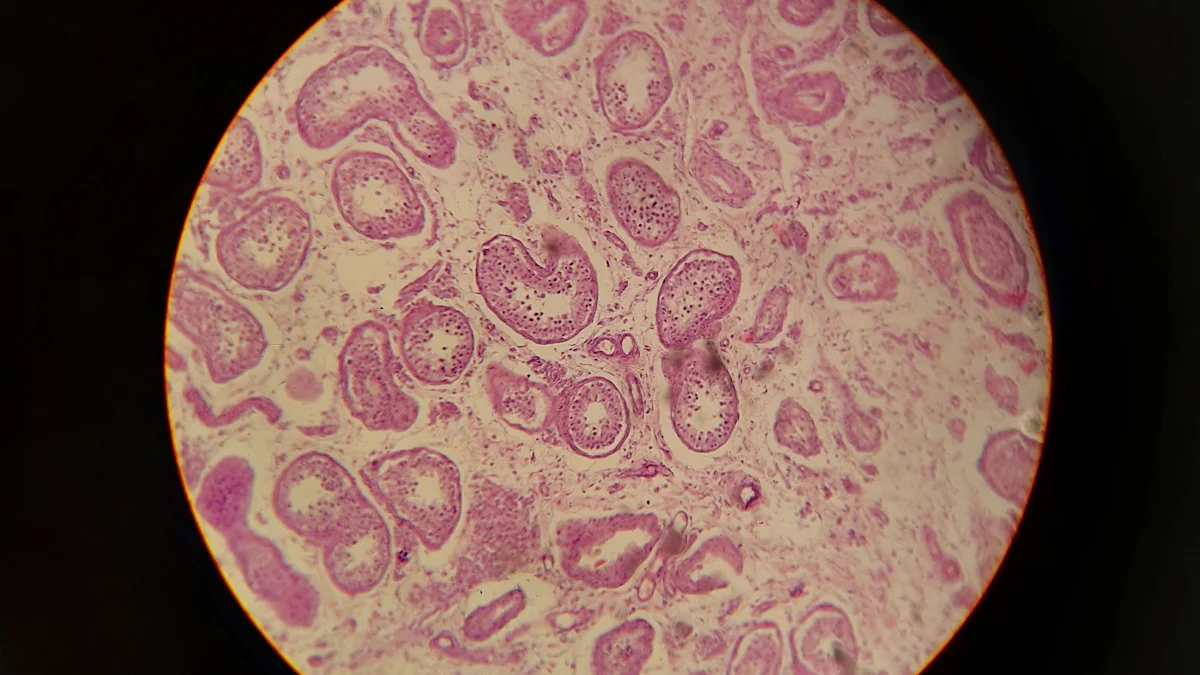
Diagnosing malignant mesothelioma at an early stage presents significant challenges:
- The disease is rare, making it less familiar to healthcare providers.
- No recommended screening tests exist for individuals without symptoms.
- Symptoms often mimic other conditions, such as pneumonia or lung cancer.
- Imaging tests frequently fail to detect early signs of mesothelioma.
Therapeutic approaches also face limitations. Standard treatments, including surgery, chemotherapy, and radiation, show modest effectiveness. Late-stage diagnosis further complicates treatment, reducing survival rates. Limited understanding of the molecular changes in malignant pleural mesothelioma hampers the development of targeted therapies. Emerging treatments, such as immunotherapy, require more research to determine their efficacy.
Role of molecular research in addressing challenges
Molecular research has significantly advanced the understanding of malignant mesothelioma. Identifying specific biomarkers has improved diagnostic accuracy and enabled the development of targeted therapies. For example, mesothelin CAR-T cell therapy, currently in clinical trials, offers a promising approach tailored to mesothelioma. Heparanase blockers and STAT3 inhibitors represent novel therapeutic strategies that could enhance treatment outcomes. Additionally, immunotherapies targeting molecular pathways provide new hope for patients. These advancements underscore the critical role of molecular research in overcoming diagnostic and therapeutic challenges.
Genetic and Epigenetic Alterations in Malignant Mesothelioma
BAP1 mutations and tumor suppression
BAP1 mutations play a critical role in the development of malignant mesothelioma. Studies reveal that 21–63% of patients carry either germline or somatic BAP1 mutations. These mutations impair tumor suppression mechanisms, leading to cancer progression. Interestingly, patients with somatic BAP1 mutations often experience longer survival rates compared to those without. Research on animal models further highlights the importance of BAP1. Mice with BAP1 mutations developed malignant mesothelioma at twice the rate of wild-type mice when exposed to asbestos. In some cases, BAP1 knockout mice developed tumors even without asbestos exposure, demonstrating the mutation’s independent role in tumorigenesis.
CDKN2A/ARF deletions and cell cycle dysregulation
The deletion of the CDKN2A/ARF locus disrupts two key tumor suppression pathways: Rb and p53. These pathways regulate the cell cycle and prevent uncontrolled cell growth. Without these mechanisms, cells proliferate uncontrollably, a hallmark of malignant mesothelioma. This deletion represents a significant genetic alteration that contributes to the aggressive nature of the disease.
NF2 mutations and Hippo pathway disruption
Mutations in the NF2 gene disrupt the Hippo signaling pathway, which regulates cell growth and organ size. Studies show that 35% of malignant mesothelioma samples contain somatic mutations in Hippo pathway genes, including NF2. The absence of key proteins like Merlin (produced by NF2) and LATS1 further confirms this disruption. These changes allow cells to bypass growth control mechanisms, promoting tumor progression.
Epigenetic changes, including DNA methylation and histone modifications
Epigenetic alterations also play a significant role in malignant mesothelioma. BAP1 inactivation affects histone modification, leading to widespread changes in gene expression. Additionally, the deletion of p16INK4a and p14ARF occurs in 80–90% of cases, highlighting the importance of DNA methylation and histone modifications in the disease. These changes alter the cellular environment, creating conditions favorable for tumor growth.
Dysregulated Signaling Pathways in Malignant Mesothelioma
Hippo pathway and its role in tumor progression
The Hippo pathway plays a pivotal role in regulating cell growth and preventing tumor progression. In malignant mesothelioma, this pathway often becomes dysregulated, leading to unchecked cellular proliferation. YAP1, a key transcriptional coactivator in the Hippo pathway, drives tumor growth when activated. Normally, the Hippo pathway phosphorylates YAP1, keeping it inactive in the cytoplasm. However, when the pathway is disrupted, YAP1 translocates to the nucleus and activates genes that promote cell survival and proliferation. This process is further amplified by TAZ, another coactivator, which works alongside YAP1 to enhance oncogenic gene expression. The loss of tumor-suppressing kinases like MST1/2 and LATS1/2 exacerbates this dysregulation, creating an environment conducive to tumor progression.
mTOR signaling and tumor growth
The mTOR signaling pathway significantly contributes to tumor growth in malignant mesothelioma by enhancing protein synthesis and ribosome biogenesis. Mutations in tumor suppressor genes, such as NF2, often activate mTORC1, a key component of this pathway. NF2-null cells exhibit sensitivity to rapamycin, an mTORC1 inhibitor, highlighting the pathway’s therapeutic potential. However, clinical trials with mTORC1 inhibitors like everolimus have shown limited success, suggesting that mTOR signaling involves complex interactions. Additionally, the loss of p19/Arf accelerates ribosome production, further driving tumor growth. These findings underscore the need for more targeted approaches to disrupt mTOR signaling effectively.
Interplay between pathways and resistance mechanisms
Interactions between signaling pathways contribute to treatment resistance in malignant mesothelioma. The PI3K/mTOR pathway plays a central role in this process. Suppressing feedback loops within this pathway often triggers the activation of compensatory mechanisms, which undermine therapeutic efficacy. For instance, inhibiting mTOR signaling can lead to the overactivation of alternative pathways, reducing the effectiveness of targeted treatments. This interplay highlights the importance of developing combination therapies that address multiple pathways simultaneously to overcome resistance and improve patient outcomes.
Mitochondrial and Metabolic Insights
Altered energy metabolism in malignant mesothelioma
Malignant mesothelioma cells undergo significant metabolic reprogramming, shifting their energy production from mitochondrial oxidative phosphorylation (OXPHOS) to glycolysis. This phenomenon, known as the Warburg effect, allows cancer cells to generate energy rapidly, even in oxygen-rich environments. Research highlights that estrogen receptor β (ERβ) activation further impairs mitochondrial respiratory chain activity, reinforcing glycolytic dependence. This metabolic shift is evident in various mesothelioma cell lines, as shown in the table below:
| Cell Line | OCR/ECAR Ratio | Glycolytic Dependence |
|---|---|---|
| H28 | Decreased | Higher dependence on glycolysis |
| H513 | Decreased | Higher dependence on glycolysis |
| H2052 | Decreased | Higher dependence on glycolysis |
| H2452 | Decreased | Higher dependence on glycolysis |
| H2596 | Decreased | Higher dependence on glycolysis |
| H2373 | Increased | Lower dependence on glycolysis |
| H2461 | Increased | Lower dependence on glycolysis |
Mitochondrial dysfunction and cancer progression
Mitochondrial dysfunction plays a pivotal role in cancer progression. Malignant mesothelioma cells exhibit altered mitochondrial shapes and functions, which influence their bioenergetics and sensitivity to treatments. Cells with low mitochondrial fractal dimension and high lacunarity show increased sensitivity to mitochondrial inhibitors like metformin and Mdivi-1. These findings suggest that mitochondrial morphology could predict the effectiveness of targeted therapies. Additionally, the dynamic nature of mitochondria underscores their importance in sustaining tumor growth and survival.
Metabolic vulnerabilities as therapeutic opportunities
Targeting metabolic vulnerabilities offers promising therapeutic opportunities for malignant mesothelioma. Disrupting mitochondrial bioenergetics through inhibitors of mitochondrial oxidoreductases, such as peroxiredoxin-3, has shown potential in reducing tumor volumes in preclinical models. Alterations in mitochondrial dynamics also present exploitable weaknesses. Therapies that target these changes could enhance treatment efficacy, particularly in patients with tumors exhibiting specific mitochondrial morphologies. These strategies highlight the potential of metabolic interventions in improving patient outcomes.
Novel Therapeutic Strategies for Malignant Mesothelioma
Targeted therapies, including BAP1 and mTOR inhibitors
Targeted therapies have emerged as a promising approach for treating malignant mesothelioma. These therapies focus on specific molecular alterations, such as BAP1 mutations and mTOR pathway dysregulation. Recent advancements include:
- PI3 kinase and mTOR inhibitors, which aim to disrupt tumor growth by targeting key signaling pathways.
- PARP blockers, which show potential when combined with platinum-based chemotherapy in BAP1-deficient tumors.
- VEGF blockers, used alongside PDL1 inhibitors, to address conditions with PDL1 upregulation.
The table below highlights some of the latest targeted therapies:
| Therapy Type | Description |
|---|---|
| PARP Blocker | Effective in platinum-sensitive conditions when combined with Ig antibody |
| VEGF Blocker | Paired with PDL1 inhibitors for PDL1-positive tumors |
| AXL Blocker | Combined with PD1 inhibitors for tumors lacking unique biomarkers |
| CDK4/6 Blocker | Designed for p16INK4A-negative conditions |
| Rucaparib | Achieved a disease control rate (DCR) of 23% and 58% at 24 and 12 weeks |
These therapies represent a significant step forward, though further research is needed to improve survival rates.
Advances in immunotherapy, including checkpoint inhibitors
Immunotherapy has revolutionized cancer treatment by harnessing the immune system to combat tumors. Checkpoint inhibitors, such as nivolumab and ipilimumab, have shown encouraging results in malignant mesothelioma. A Phase III trial combining these agents reported a median overall survival of 19.1 months and a one-year survival rate of 68%. The table below summarizes key findings:
| Trial Phase | Treatment Combination | Disease Control Rate | Median Overall Survival | 1-Year Survival Rate |
|---|---|---|---|---|
| Phase I/II | Yervoy and Opdivo | Positive results | N/A | N/A |
| Phase III | Nivolumab and Ipilimumab | Over 65% | 19.1 months | 68% |
These results highlight the potential of immunotherapy to improve outcomes for patients with advanced disease.
Combination therapies for improved outcomes
Combination therapies offer a multifaceted approach to treating malignant mesothelioma. Standard regimens, such as cisplatin with pemetrexed, remain the first-line treatment for unresectable cases. Researchers are exploring additional combinations to enhance efficacy. Antiangiogenic tyrosine kinase inhibitors (TKIs) and bevacizumab, an anti-VEGF monoclonal antibody, have shown promise in clinical studies. Immunotherapy combined with chemotherapy has also demonstrated improved prognosis by increasing lymphocyte infiltration into tumors.
The table below outlines notable combination therapies:
| Combination Therapy | Description | Evidence Source |
|---|---|---|
| Cisplatin + Pemetrexed | Standard first-line chemotherapy for malignant pleural mesothelioma | FDA approval based on EMPHACIS study |
| Antiangiogenic TKIs | Investigated alone or with standard therapy to improve outcomes | Ongoing research |
| Bevacizumab | Validated for malignant pleural mesothelioma treatment | Clinical studies |
| Immunotherapy | Linked to better prognosis through lymphocyte infiltration | Tumor-infiltrating lymphocytes studies |
These strategies underscore the importance of combining therapies to address the complexity of the disease and improve patient survival.
Future Directions in Malignant Mesothelioma Research
Personalized medicine and tailored treatments
Personalized medicine offers a transformative approach to treating malignant mesothelioma. By tailoring therapies to individual genetic and molecular profiles, researchers aim to improve treatment outcomes. For instance, combining PARP blockers with Ig antibodies has shown a disease control rate (DCR) of 23% at 24 weeks in platinum-sensitive conditions. Similarly, VEGF blockers paired with PDL1 inhibitors achieved a DCR of 58% at 12 weeks in PDL1-positive cases. The table below highlights additional personalized approaches:
| Approach | Description | Outcome |
|---|---|---|
| PARP Blocker with Ig Antibody | For platinum-sensitive conditions | DCR of 23% at 24 weeks |
| VEGF Blocker with PDL1 Blocker | For PDL1-positive conditions | DCR of 58% at 12 weeks |
| AXL Blocker with PD1 Blocker | For tumors without unique biomarkers | N/A |
| CDK4/6 Blocker | For p16ink4A-negative conditions | N/A |
| PARP Blockers | For BAP1/BRCA1-negative conditions | N/A |
These strategies emphasize the potential of precision medicine to address the unique characteristics of each patient’s disease.
Early detection and biomarker discovery
Early detection remains a critical goal in malignant mesothelioma research. Identifying reliable biomarkers can enable earlier diagnosis, improving survival rates. Promising biomarkers include ATG5, which demonstrates high sensitivity and specificity in pre-diagnostic samples. miR-222 distinguishes between asbestos-exposed individuals and those with mesothelioma. Mesothelin, a validated blood-based biomarker, holds both diagnostic and prognostic value. The table below summarizes these findings:
| Biomarker | Significance | Notes |
|---|---|---|
| ATG5 | Early detection of malignant mesothelioma | High sensitivity and specificity in samples |
| miR-222 | Promising biomarker | Differentiates asbestos exposure from disease |
| Mesothelin | Validated blood-based biomarker | Diagnostic and prognostic value for mesothelioma |
These biomarkers represent a significant step toward earlier and more accurate diagnosis.
Promising areas for future research, including epigenetic therapies
Epigenetic therapies offer a promising frontier in malignant mesothelioma research. These therapies target reversible changes in gene expression, such as DNA methylation and histone modifications. Researchers are exploring drugs that restore normal epigenetic patterns, potentially reversing tumor growth. Combining epigenetic therapies with immunotherapy or targeted treatments could enhance their effectiveness. Future studies may also investigate how epigenetic changes influence treatment resistance, paving the way for more durable responses. This area of research holds immense potential for improving patient outcomes.
Recent advancements in understanding the molecular pathogenesis of malignant mesothelioma have transformed the landscape of research and treatment. Insights into genetic alterations, such as NF2 mutations and Hippo pathway dysregulation, have clarified disease mechanisms. These discoveries have driven innovative diagnostic tools and therapies, including immunotherapies and cancer vaccines. However, challenges persist, particularly in validating experimental findings and refining treatment protocols. Continued research remains essential to address these gaps and improve patient outcomes.
FAQ
What is the primary cause of malignant mesothelioma?
Asbestos exposure is the leading cause. Inhaled fibers lodge in the pleura, causing inflammation and DNA damage, which can lead to cancer after decades.
Why is malignant mesothelioma challenging to diagnose early?
The disease mimics other conditions like pneumonia. Symptoms appear late, and no reliable screening tests exist for asymptomatic individuals.
How does molecular research improve mesothelioma treatment?
Molecular research identifies genetic mutations and biomarkers. These discoveries enable targeted therapies, immunotherapies, and personalized treatments, improving patient outcomes and survival rates.
